Abstract
Background: Pain interference and sleep problems (sleep disturbance and sleep-related impairment) are prevalent complications experienced by pediatric patients living with sickle cell disease (SCD). If sleep problems contribute to increased pain interference, sleep-directed behavioral interventions could be an additional non-opioid approach to minimizing pain in SCD patients. We hypothesized that sleep disturbance and sleep-related impairment are associated with an increase in pain interference. Second, we studied the prevalence of a later chronotype (preferred timing of sleep) and social jetlag (difference in sleep patterns during the week and weekend), which are measures of circadian sleep patterns, in pediatric patients with SCD.
Methods: We performed a IRB approved cross-sectional survey of pediatric patients with SCD aged 8-17 years at a single clinic visit using PROMIS (Patient Reported Outcomes Measurement System) pain interference, sleep disturbance and sleep-related impairment item banks, which utilize T-scores to measure the severity of these parameters; greater scores in each domain signify greater severity. The µMCTQ (ultra-short Munich Chronotype Questionnaire) assessed mid-sleep time (a proxy for chronotype) and social jetlag. Analyses were performed to assess associations between PROMIS measures, sleep patterns and clinical variables using JMP Pro16 (Cary, NC).
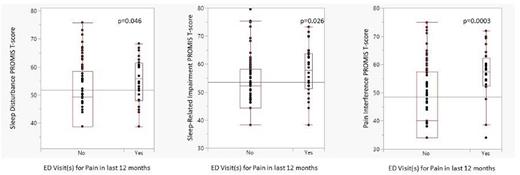
Results: One hundred and five patients (mean age: 13.1±2.6 years; 53 male, 52 female) completed the PROMIS sleep and pain measures. All participants approached completed the PROMIS evaluation for pain and sleep. The majority of patients (81.9%) were diagnosed with either HbSS or HbSβ0 -thalassemia and 61% were on hydroxyurea (alone or with an additional sickle cell modifying therapy). Pain interference was significantly associated with both sleep disturbance (r=0.49, p<0.0001) and sleep-related impairment (r=0.46, p<0.0001). In multivariate analysis for pain interference, both sleep disturbance (p=0.0007) and sleep-related impairment (p=0.006) remained in the model. Females participants reported higher T-scores for sleep-related impairment than males (females: 56.7± 10 vs males 50.2± 9.4, p=0.0009). Patients with one or more ED visits for pain in the last year reported greater sleep disturbance (55.0±8.5 vs 50.7± 10, p=0.046) and sleep-related impairment (57.1± 9.3 vs 52.1± 10.2, p=0.026) (Figure). The average mid-sleep time (clock time) was 4:14 ± 1:44 AM and the average social jetlag (hh:mm) was 2:32 ± 1:35.
Conclusion: Pain interference is associated with both sleep disturbance and sleep-related impairment and our 100% acceptance rate for completing PROs highlights the clinical importance of performing formal sleep and pain assessments. A longitudinal examination of sleep and pain in pediatric SCD patients is needed to determine if sleep problems and pain have a bi-directional relationship. Furthermore, the high prevalence of later mid-sleep times and social jetlag in this sample suggests that longitudinal studies should incorporate measures of sleep timing and social jetlag impact on pain.
Disclosures
Ilonze:Global Blood Therapeutics: Consultancy. Lebensburger:Novartis: Consultancy; Forma Therapeutics: Consultancy; BPL: Consultancy; Agios Pharmaceuticals: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal